Lydia Cahyatrianti DVM, CVA
Makassar Pet Clinic, Makassar, South Sulawesi, Indonesia
History
A 2-year-old, neutered male domestic short hair cat, with a playful temperament, suddenly began dragging his hind limbs. Upon examination, it was found he had been shot with a lead bullet on the lumbar (Figure 1) and needed
surgery to remove it. Surgery was performed to take the bullet out, and the owner informed that the spinal cord was torn. Two weeks post-surgery, he still couldn’t walk by himself, exhibited pain when touched, lacked appetite, and couldn’t control urination and defecation. The owner was devastated and wanted a better quality of life even though she knew that he couldn’t walk normally. Acupuncture treatment was suggested.
Western Examination
Upon presentation, a neurological examination was performed. The cat was non-ambulatory and seemed depressed. He had an open wound at the lumbar area. Both the front limbs showed normal spinal reflex on examination. Proprioceptive placing for the hind limbs was absent, and Panniculus reflexes were negative from lumbar to the caudal area. Patellar and withdrawal reflexes were also negative, as was deep pain.
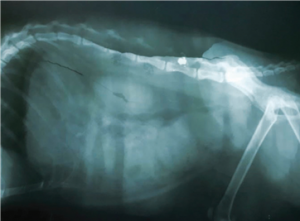
| Figure 1: Lateral view radiograph of lumbar area of 2-year old cat showing a lead bullet inside the spinal canal. |
His tail was paralyzed and perineal reflex was negative. The muscle tone of the hind limbs was absent and had started to atrophy. He was graded 5 on neurological deficit.
TCVM Examination and Diagnosis
The cat’s tongue was purple and wet, his ears felt cold, and his pulse was deep, slow and weaker on the right side. The purple tongue indicated Stagnation and wetness indicated Cold. Pulse was deep, slow and weaker on the right side, indicating Qi or Yang deficiency.1 His back felt cold and very sensitive on Spleen Shu and Mu point (BL-20 and LIV-13), Kidney Shu point (BL23),1 Bai Hui point, and almost all of the Bladder Channel.
The TCVM diagnoses included lumbar spinal cord Qi-Blood Stagnation leading to Kidney Yang and Qi Deficiency with Spleen Qi Deficiency. The Eight Principles method of TCVM showed an Interior Pattern. Spinal Cord Qi-Blood Stagnation is always an Interior Pattern and Cold makes it Yang Deficiency. The Zang-Fu organs affected were Kidney and Spleen. The Meridians involved included Kidney, Bladder, and Spleen.
TCVM Treatment
The treatment aimed to remove Stagnation and tonify Yang and Qi deficiency. Initial treatment was done with dry needle acupuncture (DNAP) on GV-20 and BL-35 for 20 minutes. Then after three days, a combination of DNAP on GV-20, Liu Feng, LIV-3, and electro-acupuncture at 20Hz was used for 10 minutes on BL-11, BL-35, KID-1, BL-40, BL-54, ST36, and SP-6 as the master points for back problems, pelvic limb paralysis, muscle atrophy and as general Qi tonic.2 Laser acupuncture was also performed on GV-1, Bai Hui, GV-3, GV4, BL-20, BL-23, Hua Tuo Jia Ji, Shen Peng, Shen Shu, and Wei Jie. The cat received twice weekly treatments for one month which were then reduced to once a week. He would lie quietly and sometimes purr as the treatments were given. In addition, the Chinese medicine herbal formulas Xiao Huo Luo Dan and Bu Yang Huan Wu were given twice daily, one capsule of 250 mg eacha. Xiao Huo Luo Dan was indicated for Bi syndrome with pain in joints or back. Bu Yang Huan Wu was indicated for Qi deficiency with Blood Stasis blocking the Channels with signs of hemiparesis or hemiparalysis such as atrophy and weakness of the hind limbs.3
Discussion
The lead bullet that damaged the spinal cord was surgically removed. This procedure was then followed by treatment (acupuncture, Chinese herbal medicine) based upon the TCVM Patterns diagnosis in the cat. This resulted in progress, even though treatment didn’t fully restore the patient to his pre-injury mobility. The cat finally could control urination and defecation. He looked happier, and his appetite increased, and he was willing to interact with other cats. The cat was fitted with a wheelchair to help him at home and allow some mobility (Figure 2).
The patient responded well to treatment and the owner remained positive with the clinical progress. The owner brings him for maintenance AP treatments every month, and the cat continues to enjoy his acupuncture treatments. The combination of Western medicine that include the surgery and TCVM treatments resulted in progress. Even though treatment didn’t fully restore the patient to his pre-injury normality, it improved his quality of life.

Figure 2: The cat using a wheelchair after acupuncture and herbal therapy for hindlimb paralysis.
Acknowledgements
This case was submitted to Chi University-Indonesia as part of the requirements to become a Certified Veterinary Acupuncturist. Due to limited space in the newsletter, this case report was shortened. For additional details on the case, please contact Dr. Lydia Cahyatrianti at l.cahyatrianti@gmail.com.
Footnotes
- PT. Primax Asia, North Jakarta City, Indonesia.
References
- Xie H, Priest V. Traditional Chinese Veterinary Medicine: Fundamental Principles, 2nd Ed. Reddick, FL: Chi Institute Press 2013: 212, 239, 246, 247, 270.
- Xie H, Priest V. Xie’s Veterinary Acupuncture. Ames, IA: Blackwell Publishing 2007: 148, 151, 163-167, 169, 190, 195, 198, 224-226, 234.
- Xie H, Priest V. Xie’s Chinese Veterinary Herbology. Ames, IA: Blackwell Publishing 2010: 457-458, 491-492.

